Government guidelines on restricting dietary fat and saturated fat to reduce cholesterol and heart disease are bad for health according to evidence from independent studies Dr. Mae-Wan Ho
The mantra that saturated fat is bad for you and must be removed to reduce the risk of heart disease has been drummed into public consciousness for almost four decades. But independent scientific evidence shows that this advice has paradoxically increased our cardiovascular risk. And the obsession with total cholesterol levels has led to the over- medication of millions with statins with yet more harm than benefit.
The British Medical Journal (BMJ) re-opened the debate on dietary fat and cholesterol lowering drugs with major articles published in October 2013, especially one by cardiologist Aseem Malhotra at Croydon University Hospital, London on why saturated fat is not the major issue [1], and another by John Abramson at Harvard Medical School and three colleagues in US and Canada universities asking if people at low risk of cardiovascular disease should take a statin [2]. The articles were in anticipation of UK’s pharmaceutical regulatory agency NICE’ new guideline issued in July 2014, which recommends statins for healthy people with a 10 % or greater ten-year risk of cardiovascular disease (CVD) [3], a dramatic change over its previous 2006 guideline, which recommended statin only for people who already had clinical CVD and whose ten-year risk of developing CVD was 20 % or greater, or whose risk was increased because of diabetes, or by being in high-risk ethnic groups. The new guidelines increased the number of people eligible for statins by 4.5 million [4]. The move followed a revision in US guideline calling for treatment of people with a 7.5 % or greater ten-year risk, which expanded the number of healthy people for whom statins were prescribed by ~13 million.
The demonization of saturated fat began with Ancel Keys’ seven countries study [5] which found a correlation between heart disease and total cholesterol concentration that in turn correlated with the proportion of energy provided by saturated fat. However, Keys excluded data from 16 countries; and when data from all the countries were included, the association between fat calories as a percentage of total calories and death from degenerative heart disease was greatly diminished, and there was no association between dietary fat and mortality from all causes [6].
Nevertheless, people were advised to cut fat intake to 30 % of total energy and saturated fat to 10 %. Dietary fat is believed to have the greatest influence on cardiovascular risk through elevated concentrations of low density lipoprotein (LDL) cholesterol [1]. But the reduction in LDL cholesterol from reducing saturated fat intake appears to be specific to large, buoyant type A LDL particles, when it is the small dense type B particles – responsive to carbohydrate intake – that are implicated in cardiovascular disease.
Recent prospective cohort studies have not supported any significant association between saturated fat intake and cardiovascular risk. If anything, saturated fat has been found to be protective in many studies.
A randomized control trial published in 2008 showed that a low carbohydrate diet gives greater improvements to health than a low fat diet with the same number of calories [7]. Several other randomized trials published between 2003 and 2007 also showed that a low carbohydrate diet reduces weight and improves lipids more than a low fat diet. Cardiovascular research scientist James DiNicolantoio commented in his review [8], that the data suggest the current global epidemic of atherosclerosis, heart disease, diabetes, obesity and the metabolic syndrome is being driven by a diet high in carbohydrate/sugar as opposed to fat.
A study published in 2012 similarly showed that a low fat diet results in the greatest decrease in energy expenditure, an unhealthy lipid pattern, and increased insulin resistance in comparison with a low carbohydrate and low glycaemic index diet [9].
As Malhotra pointed out [1], food with most of the fat removed generally does not taste as good. To compensate, the food industry puts in more sugar. Scientific evidence is mounting that sugar is a possible independent risk factor for the metabolic syndrome (the cluster of hypertension, dysglycaemia, increased triglycerides, low HDL (high density lipid) cholesterol, and increased waist circumference). In previous generations, cardiovascular disease existed largely in isolation. Today, two-thirds of people admitted to hospital with diagnosed acute myocardial infarction have metabolic syndrome, and 75 % have completely normal total cholesterol concentrations.
Malhotra drew attention to several independent population studies in healthy adults, which have shown that low total cholesterol is associated with cardiovascular and non-cardiac mortality, indicating that high total cholesterol is not a risk factor in healthy populations [1].
Among the most recent is a community-based prospective cohort study in 12 rural areas in Japan involving 12 334 healthy adults aged 40 to 69 years, who were screened for serum total cholesterol. The outcome measured was total mortality by sex and cause of death, with average follow-up period of 11.9 years [10].
The results showed that compared with a moderate cholesterol level of 4.14 – 5.17 mmol/L, the age-adjusted hazard ratio (HR) of low cholesterol (< 4.14 mmol/L) was 1.49 (95 % confidence interval (CI) 1.23-1.79) in men and 1.50 (95 % CI 1.10-2.04) in women. High cholesterol (≥6.21 mmol/L) was not a risk factor. The association remained almost the same in analyses that excluded deaths due to liver disease. The multivariate-adjusted HRs and CIs of the lowest cholesterol group for haemorrhagic stroke, heart failure (excluding myocardial infarction) and cancer mortality are significantly higher than those of moderate cholesterol group for each cause of death. The current UK and US recommended normal level of cholesterol is <5 mmol/L.
National dietary guidelines were first introduced in 1977 and 1983 by US and UK government respectively, to reduce coronary heart disease (CHD) by reducing fat intake. But no analysis of the evidence base for the recommendations has ever been undertaken. A new study examines the evidence from randomized controlled trials (RCTs) available to the US and UK regulatory committees at their respective points of implementation. A team led by Zoë Harcombe at the University of the West of Scotland, Hamilton carried out a systematic review and meta-analysis on RCTs published prior to 1983 on the relationship between dietary fat, serum cholesterol and the development of CHD [11]. A total of 2 467 males participated in 6 dietary trials consisting of 5 secondary prevention studies and one that included healthy participants.
There were 370 deaths from all causes in both the intervention and control groups. The risk ratio (RR) from meta-analysis was 0.996 (CI 0.865 to 1.147). There were 207 and 216 deaths from CHD in the intervention and control groups respectively, the RR was 0.989 (95 % CI 0.784 to 1.247). There were no significant differences in death from all causes or from CHD between intervention and control groups.
The mean serum cholesterol levels fell in all groups, control and intervention. The standardized mean different for the six trials combined was -12.6 % + 6.7 % for the intervention groups and -6.5 % + 5.1 % for the control groups. Though significantly higher in the intervention groups, this did not result in significant difference in death from CHD or from all causes.
The authors concluded [11, p.6]: “It is a widely held view that reductions in cholesterol are healthful per se. The original RCTs did not find any relationship between dietary fat intake and deaths from CHD or all-causes, despite significant reduction in cholesterol levels in the intervention and control groups. This undermines the role of serum cholesterol levels as an intermediary to the development of CHD and contravenes the theory that reducing dietary fat generally and saturated fat particularly potentiates a reduction in CHD.” Finally, they stated: “The present review concludes that dietary advice not merely needs review; it should not have been introduced.”
What about replacing saturated fat with polyunsaturated fat? RCTs of mixed W-3 and W-6 polyunsaturated fatty acids (PFUAs) (see Box) and meta-analysis of their coronary heart disease (CHD) outcomes have been deemed decisive evidence for the advice to consume at least 5-10 % of energy as W-6 PFUAs by the American Heart Association. But the conclusions of those meta-analyses have been criticized for omission of relevant trials with unfavourable outcomes, inclusion of trials with weak design and dominant confounders, failure to distinguish between trials that selectively increased W-6 PFUAs from those that substantially increased W-3 PFUAs, and failure to acknowledge that W-3 and W-6 PFUAs replaced large quantities of trans-fatty acids (TFAs) - generally acknowledged to be bad for health - in addition to saturated fatty acids (SFAs) in several trials.
A team led by Christopher Ramsden at National Institutes of Health Bethesda, Maryland in the US carried out a fresh meta-analysis of the RCTs involving dietary interventions with W-3 and W-6 PUFAs [12]. Nine trials were identified by literature search and review of public records, including one that was not in previous meta-analyses. Two trials were excluded because the patients were not randomized as individual patients. The remaining seven RCTs with 8 datasets totalling 11 275 subjects were included in the main analysis.
For non- fatal myocardial infarction (MI) and death from coronary heart disease (CHD), the pooled risk reduction for mixed W-3 and W-6 PFUAs was 22 % (risk ratio (RR) 0.78, CI 0.65-0.93) compared to an increased risk of 13 % for W-6 PFUAs specific diet (RR 1.13, CI 0.84-1.53). RCTs that substituted W-6 PFUAs for TFAs and SFAs without simultaneously increasing W-3 PFUAs increased risk of death that approached statistical significance: RR 1.16, CI 0.95-1.42. The authors concluded [12] that advice to specifically increase W-6 PFUAs intake is unlikely to provide the intended benefits and may actually increase the risks of CHD and death.
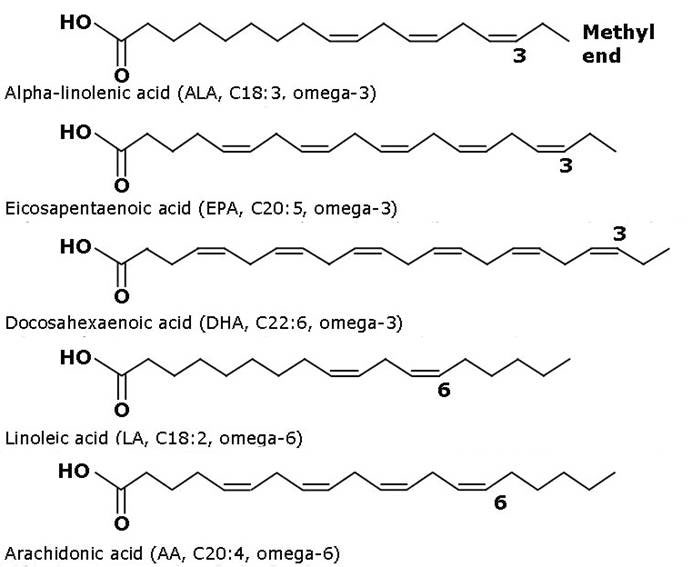
A fatty acid is a carboxylic acid with a long hydrocarbon chain that is either saturated (with no double bonds between carbon molecules in the chain) or unsaturated with one or more double bonds between carbon molecules in the chain). Polyunsaturated fatty acids have more than one double bond in the chain. W-3 and W-6 polyunsaturated fatty acids refer to the position of the last double bond in the chain (see Figure).
In an uptake, Ramsden and colleagues recovered data from Sydney Diet Heart Study using W 6 PUFAs in secondary prevention of CHD, and updated meta-analysis [13]. The participants were 458 men aged 30-59 years with a recent coronary event. The intervention involved replacing dietary saturated fats (from animal fats, common margarines, and shortenings) with W 6 linoleic acid from safflower oil and safflower oil polyunsaturated margarine. Controls received no specific dietary instruction or study foods.
The intervention group (n=221) ended up with higher death rates than controls (n=237): death from all causes 17.6 % vs 11.8 %, HR 1.62 (CI 1.00-2.64); death from cardiovascular disease 17.2 % vs 11.0 %, HR 1.7 (CI 1.03-2.8); death from coronary heart disease 16.3 % vs 10.1 %, HR 1.74 (CI 1.04-2.92).
Including the recovered data in an updated meta-analysis of linoleic acid intervention trials showed non-significant trends toward increased risks of death from coronary heart disease (HR 1.33 CI 0.99 to 1.79); P=0.06) and cardiovascular disease (HR 1.27 CI 0.98 to 1.65); P=0.07).
Current government guidelines on dietary fat are not supported by independent evidence from randomized control trials. First, there is no association between heart disease, blood cholesterol and dietary fat; and a meta-analysis of the RCTs available at the time the first guidelines were introduced confirmed that there was no relationship between dietary fat intake and deaths from CHD or all-causes, despite significant reduction in cholesterol levels in the intervention and control groups. Second, low fat diets (in accordance with government guidelines) are actually bad for health in comparison with low carbohydrate, low glycaemic diets of the same calorific content. Third, independent population studies showed that while low cholesterol level is a significant risk factor for cardiovascular and non-cardiac mortality in healthy individuals, high cholesterol level is not. Finally, the advice to specifically increase W-6 PFUAs intake may actually increase the risks of CHD and death.
In view of this evidence on the lack of association between heart disease, blood cholesterol and dietary fat, the mass medication of healthy people with cholesterol lowering statins has resulted in yet more harm than good (see [14] Statins for the Healthy are Harmful, SiS 66).
Article first published 13/04/15
Comments are now closed for this article
There are 7 comments on this article.
www.gold-dna.de Comment left 14th April 2015 01:01:19
And do not forget the connection between cholesterol and vitamin D. Without the former there is no later, even if you are in the sun with bare skin for hours ...
Dr Anthony Smith Comment left 14th April 2015 01:01:08
There is a large volume of research/information/trials going back many years showing the most important factor regarding dietary fat is the ratio between omega6 and omega3. In theory this ratio should be close to 1:1, but in fact in western diets due to the wholesale use of vegetable oil (LA), the ratio is heavily in favour of omega6. This adverse ratio is linked to proinflammatory states and implicated in cardiovascular disease, cancer and the many autoimmune disorders.
Sugar, salt, transfat and Linoleic acid are the major problems.
Peter K Comment left 14th April 2015 16:04:55
I don't know all the facts and can only infer. But an expansion of the market for statins by 4.5m in UK and 13M in U.S. will have big Pharma salivating. Given the lobbying power of the industry, how do we ensure objectivity and transparency in regulation, and accountability for policy?
james Comment left 14th April 2015 16:04:40
There another issue with low cholesterol and low saturated fat, and it has less to do with heart disease than neurodegenerative diseases. Deficiencies in either cause serious problems in the glia connectome, our super brain that is in charge of our central nervous system. Polyunsaturated fatty acids are highly inflammatory and prone to oxidation. With our microglia activated all the time, they become asthenic(weak), they have to divide too often, get shorter and shorter telomeres and eventually become part of the problem when they cannot clear away fast enough the amyloid beta that is normally being used in breaking down pyruvate. Amyloid-beta has the unique capability of stimulating the production of an enzyme, lactate dehydrogenase, which promotes the breakdown of pyruvate into lactate, through an anaerobic fermentation process, rejuvenating NAD+ and enabling the further production of a substantial amount of ATP through additional glycolysis. Lack of enough sat fat and cholesterol jeopardizes this whole process and the mitochondria end up producing too much ROS. etc.etc.
Mae-Wan Ho Comment left 14th April 2015 18:06:30
Thank you all for excellent information provided. The focus on single measure, cholesterol in the case of cardiovascular health, is typical of reductionist medicine, ignoring the fact that cholesterol metabolism is intimately connected with steroid biosynthesis, and is an essential component of cell membranes. Worse yet, statins target a major metabolic enzyme HMG-CoA reductace which produces mevalonate, way up in a cascade of reactions that eventually produces cholesterol, and includes the synthesis of steroid hormones as well as vitamin D from cholesterol.
Todd Millions Comment left 19th April 2015 15:03:40
Where any correlations between Hydrolysed -oils(waxes),and health done? Cardio in particular,and cotton-seed oil at top of the list.
I never bought the cholesterol link-it digests and solvents(in a bowl) upon application of vegetable acids too easily.
Beata Badzioch Comment left 26th July 2015 15:03:28
HDL(High-density lipoprotein)composed of multiple proteins transport all fat molecules (lipids), such as cholesterol, phospholipids and triglycerides around the body within the water outside cells and into the bloodstream, out of artery walls, so nicknamed "good cholesterol". LDL (Low-density lipoprotein) transport the same lipids into cells and to macrophages in the wall of arteries, nicknamed "unhealthy cholesterol",because if in excess of it causing myocardial infarction.There are many studies proving lack and unknown of this disease in the nations feeding with plant base fats. Excess of carbohydrates is the specific watch to diabetic inclinations as it is connected with insulin. In conclusion the care needs to be individualized to body problems and needs that can be so different among many individuals. In other words 2 individuals with exactly the same diet may not have the same health and strength. However to be on the good side food producing lots of vitamins and minerals so helping in digestion of other food is the best.